24 Jun 2024
Percutaneous coronary intervention for bifurcation coronary lesions using optimised angiographic guidance: the 18th Consensus Document from the European Bifurcation Club
Selected in EuroIntervention by A. N. Calik , H. Kadıoğlu
In coronary bifurcation lesions (CBL) PCI, intracoronary imaging (ICI) is preferred for its superior outcomes over angiography alone, but its adoption is limited by education and technology access barriers, resulting in most CBL PCIs still using angiographic guidance only.
References
Authors
Francesco Burzotta, Yves Louvard, Jens Flensted Lassen, Thierry Lefèvre, Gérard Finet, Carlos Collet, Jacek Legutko, Maciej Lesiak, Yutaka Hikichi, Remo Albiero, Manuel Pan, Yiannis S. Chatzizisis, David Hildick-Smith, Miroslaw Ferenc, Thomas W. Johnson, Alaide Chieffo, Olivier Darremont, Adrian Banning, Patrick W. Serruys, Goran Stankovic
Reference
DOI: 10.4244/EIJ-D-24-00160
Published
MAY 16, 2024
Link
Read the abstractReviewers
Our Comment
Why this document - the rationale/objective?
In this year's annual European Bifurcation Club (EBC) meeting, intracoronary imaging (ICI) in coronary bifurcation lesions (CBLs) was a major focus. However, concerns about reimbursement issues and inadequate education to interpret ICI-provided images limit the widespread utilization of ICI.
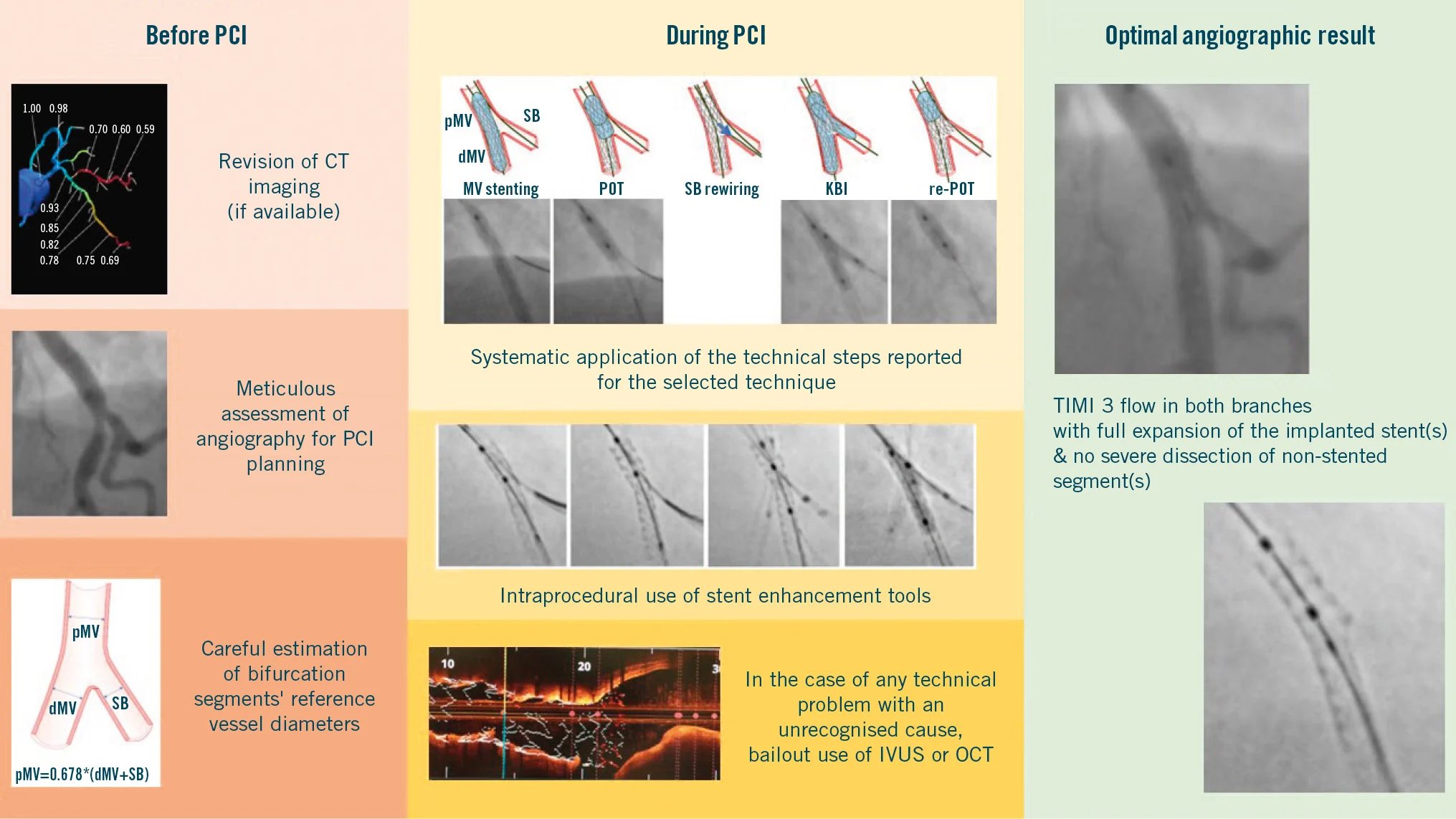
As a result, the EBC committee has decided to create a consensus document that discusses optimal angiographic guidance, steps, tips, and tricks for situations when ICI is not available (Figure 1).
Figure 1: Key points for achieving an optimal angiography-guided PCI. The key points for achieving an optimal angiography-guided PCI include a thorough analysis of pre-PCI images (computed tomography angiography, multiple angiographic views, quantitative coronary angiography vessel estimation), a systematic application of the technical steps suggested for a given selected technique, an intraprocedural or post-PCI use of stent enhancement and a low threshold for bailout use of intravascular imaging. CT: computed tomography; dMV: distal main vessel; IVUS: intravascular ultrasound; KBI: kissing balloon inflation; MV: main vessel; OCT: optical coherence tomography; PCI: percutaneous coronary intervention; pMV: proximal main vessel; POT: proximal optimisation technique; SB: side branch; TIMI: Thrombolysis in Myocardial Infarction Source: EuroIntervention Journal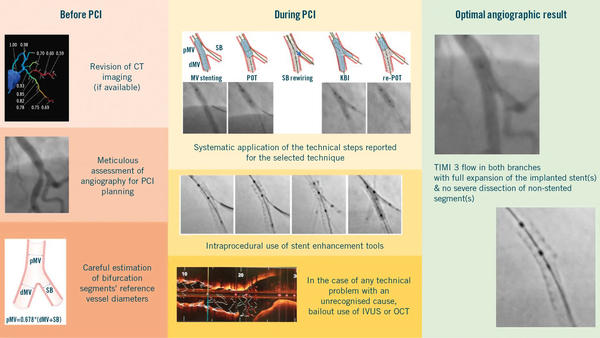
How to approach a bifurcation PCI in the absence of ICI?
The recommendation of EBC emphasizing the importance of simplifying and standardising the procedure as much as possible and limiting the number of implanted stents by using a stepwise provisional strategy1 has been further supported by the long-term results of the EBC TWO (non-left main)2 and EBC MAIN (left main)3 trials, and remains the recommended strategy for the majority of true LM and non-LM CBLs.
The objective of angiography-guided bifurcation PCI is to attain "procedural success," which involves correctly positioning the stent(s) in the bifurcation segments and ensuring optimal expansion of the implanted stents while avoiding procedural angiographic complications like underexpansion, malapposition, dissection and thrombosis that could result in adverse clinical outcomes4.
To avoid stent underexpansion and malapposition, high-pressure balloon post-dilatation of all stented segments of the coronary bifurcation is recommended1. This includes extensive use of non-compliant balloons in both 1- and 2-stent techniques and the systematic performance of high-pressure final kissing balloon inflation (KBI) in 2-stent techniques.
A new technique involves injecting a small amount of contrast during stent post-dilatation to identify balloon undersizing in angiography-guided procedures. The "distal puff sign", where contrast bypasses the inflated balloon, indicates significant malapposition between the stent/balloon and vessel wall. This is referred to as the "POT-puff sign" when observed during POT5.
Coronary CTA: what can we derive from it?
The consensus document strongly recommends to thoroughly examine the CTA images (if available) before performing CBL and LM percutaneous PCI.
Briefly, a careful CTA analysis can provide the operators with the following data:
- The 3D nature of CT can assist in identifying the optimal angiographic view.
- Non-calcified plaques in the pMV or SB with low attenuation has been shown to predict SB occlusion, while calcium presence in the contralateral side of the bifurcation can affect stent expansion and symmetry, predicting carina shift. CCTA provides detailed data on calcified plaques similar to ICI.
- FFRCT is a non-invasive method to evaluate blood flow in coronary lesions, aiding in ischemia detection and pre-PCI assessment, including virtual stenting options.
How to determine reference vessel sizes by angiography?
The consensus document emphasizes the challenges of estimating vessel size accurately with angiography because of its inherent limitations due to two-dimensional (2D) nature. To address this issue, specialized 2D and 3D quantitative coronary angiography (QCA) analysis software designed for bifurcation cases has been developed and is highly recommended for use6.
Measurements obtained from intravascular ultrasound (IVUS) and optical coherence tomography (OCT), with OCT offering superior resolution, are considered the gold standard for determining vessel sizes in coronary interventions. These measurements typically yield larger dimensions compared to those derived from quantitative coronary angiography (QCA).
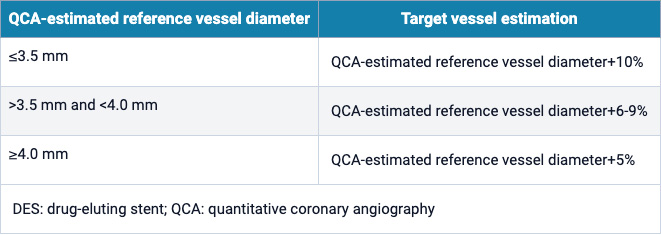
In a recent prospective, randomized GUIDE-DES trial7, an adjusted angiographic stent-sizing approach was introduced. The trial encompassed bifurcation lesions and two-stent strategies, and compared adjusted-QCA sizes based on angiographic vessel measurements to those obtained from ICI. The findings aimed to provide guidance on stent sizing for optimal outcomes in various coronary intervention scenarios (Table 1).
Table 1: Target diameters of the reference segments obtained by adjusting QCA values in the GUIDE DES trial. Source: EuroIntervention Journal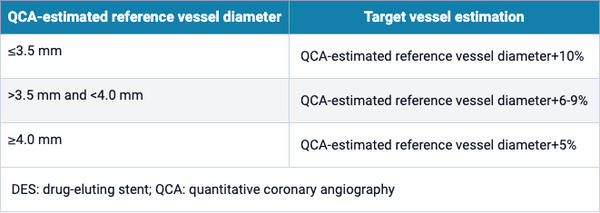
What is new with stent selection and deployment?
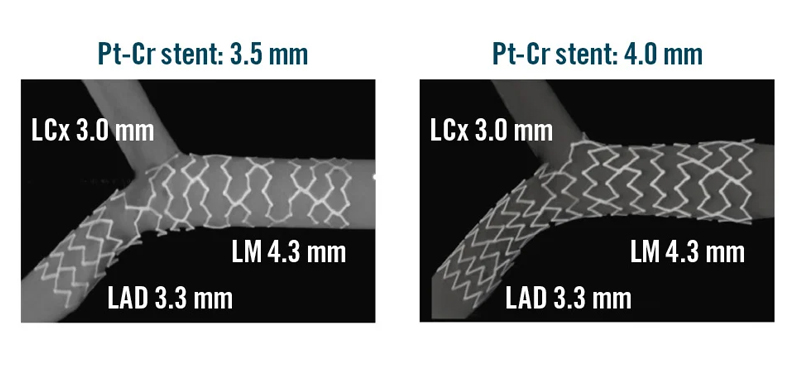
A recent innovative concept of stent under-deployment has emerged, suggesting potential benefits in stent deployment strategies. Hikichi et al. introduced a study demonstrating that selecting a stent platform based on the proximal main vessel (pMV) size can lead to a more favorable stent configuration. In their research, the authors opted for a stent based on the pMV size and intentionally under-deployed it in the distal main vessel (dMV) by inflating below nominal pressures.
Subsequently, they performed post-dilation on the proximal portion using a non-compliant (NC) balloon. This approach is particularly recommended in cases of significant size discrepancies and for Medina 0,0,1 lesions.
Bench studies have shown that this technique results in improved stent coverage and apposition, highlighting its potential advantages in certain coronary intervention scenarios8,9 (Figure 2).
Figure 2: Bench test comparison of final stent conformation obtained by provisional stenting using two different stent platforms by the same manufacturer. A) SYNERGY (Boston Scientific) 3.5 mm×20 mm DES implanted at nominal pressures followed by POT and kissing. B) SYNERGY (Boston Scientific) 4 mm×20 mm DES implanted at low pressure followed by POT and kissing. Cr: chromium; DES: drug-eluting stent; LAD: left anterior descending artery; LCx: left circumflex artery; LM: left main artery; POT: proximal optimisation technique; Pt: platinum Source: EuroIntervention Journal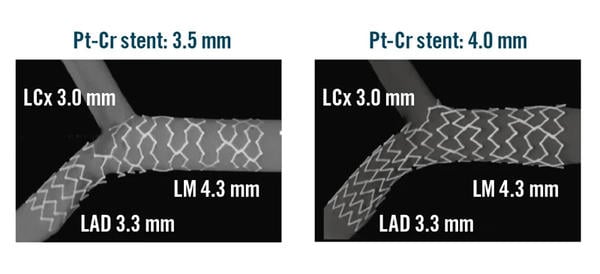
Assessment of stent conformation in the absence of ICI
ICI plays a crucial role in allowing operators to identify and rectify any procedural errors. For instance, ICI enables assessment of distal rewiring in non-DK crush techniques and non-distal rewiring in DK-crush, as well as evaluation of abluminal wiring and stent apposition/expansion.
In cases where ICI is not available, alternative methods can be utilized to assess key steps:
- The "POT-puff sign’’ (Please see the 2nd section of the review above).
- Stent enhancement technology offers an additional means to assess stent configuration and rewiring sites. Although this technique may lead to increased radiation exposure, particularly without ICI, it offers crucial procedural guidance and optimization data.
Conclusion
To conclude, in CBL PCI, ICI is increasingly recognized as the preferred guidance method due to its superior outcomes compared to angiography alone. However, widespread adoption of ICI is hindered by education and technology access barriers, leading to the majority of CBL PCIs worldwide being performed with angiographic guidance only.
The key elements for achieving optimal angiography-guided PCI, as depicted in the central illustration, include thorough pre-PCI image analysis (CTA, multiple angiographic views, QCA vessel estimation), methodical application of recommended technical steps for a selected technique, consideration of stent enhancement during or after the procedure, and a proactive approach to using intravascular imaging when needed.
References
- Burzotta F, Lassen JF, Lefèvre T, Banning AP, Chatzizisis YS, Johnson TW, Ferenc M, Rathore S, Albiero R, Pan M, Darremont O, Hildick-Smith D, Chieffo A, Zimarino M, Louvard Y, Stankovic G. Percutaneous coronary intervention for bifurcation coronary lesions: the 15th consensus document from the European Bifurcation Club. EuroIntervention. 2021;16: 1307-17.
- Arunothayaraj S, Behan MW, Lefèvre T, Lassen JF, Chieffo A, Stankovic G, Burzotta F, Pan M, Ferenc M, Hovasse T, Spence MS, Brunel P, Cotton JM, Cockburn J, Carrié D, Baumbach A, Maeng M, Louvard Y, Hildick- Smith D. Stepwise provisional versus systematic culotte for stenting of true coronary bifurcation lesions: five-year follow-up of the multicentre ran- domised EBC TWO Trial. EuroIntervention. 2023;19:e297–304.
- Hildick-Smith D, Egred M, Banning A, Brunel P, Ferenc M, Hovasse T, Wlodarczak A, Pan M, Schmitz T, Silvestri M, Erglis A, Kretov E, Lassen JF, Chieffo A, Lefèvre T, Burzotta F, Cockburn J, Darremont O, Stankovic G, Morice MC, Louvard Y. The European bifurcation club Left Main Coronary Stent study: a randomized comparison of stepwise provisional vs. systematic dual stenting strategies (EBC MAIN). Eur Heart J. 2021;42:3829-39.
- Lunardi M, Louvard Y, Lefèvre T, Stankovic G, Burzotta F, Kassab GS, Lassen JF, Darremont O, Garg S, Koo BK, Holm NR, Johnson TW, Pan M, Chatzizisis YS, Banning AP, Chieffo A, Dudek D, Hildick-Smith D, Garot J, Henry TD, Dangas G, Stone G, Krucoff MW, Cutlip D, Mehran R, Wijns W, Sharif F, Serruys PW, Onuma Y. Definitions and Standardized Endpoints for Treatment of Coronary Bifurcations. EuroIntervention. 2023;19:e807-31.
- Aminfar F, Rubimbura V, Maillard L, Noble S, Rangé G, Belle L, Derimay F, Bellemain-Appaix A, Al Karaky A, Morelle JF, Sideris G, Motreff P, Muller O, Adjedj J. The POT-PUFF sign: an angiographic mark of stent malapposition during proximal optimisation. EuroIntervention. 2023;18: 1456-7.
- Grundeken MJ, Ishibashi Y, Ramcharitar S, Tuinenburg JC, Reiber JH, Tu S, Aben JP, Girasis C, Wykrzykowska JJ, Onuma Y, Serruys PW. The need for dedicated bifurcation quantitative coronary angiography (QCA) software algorithms to evaluate bifurcation lesions. EuroIntervention. 2015;11 Suppl V:V44-9.
- Lee PH, Hong SJ, Kim HS, Yoon YW, Lee JY, Oh SJ, Lee JS, Kang SJ, Kim YH, Park SW, Lee SW, Lee CW; GUIDE-DES Trial Research Group. Quantitative Coronary Angiography vs Intravascular Ultrasonography to Guide Drug-Eluting Stent Implantation: A Randomized Clinical Trial. JAMA Cardiol. 2024;13:e240059.
- Y. Hikichi. Importance of stent selection in LMT Bifurcation stenting – Insights from the bench test, distal low pressure dilatation technique. EBC meeting. 13 Oct 2023. Warsaw, Poland.
- Burzotta F, Aurigemma C, Paraggio L, Romagnoli E, Leone AM, Vergallo R, Cangemi S, Bianchini F, Trani C. Under-deployment of extra- large drug-eluting stent: an adapted provisional technique for selected patients with distal lesions in large left main. Minerva Cardiol Angiol. 2023;71:20-6.







1 comment
It is an interesting concept and one that part ways with the common sense and careful use of a stent based on the distal vessel diameter as a protective measure towards distal dissections. But I do not think it can be used as a rule. Contrary to what is said, I would probably be more inclined to use this approach in cases where the bunch of the plaque is in the main vessel, not in the daughter branch. But there are so many difference from case to case based on the compliance of the vessel, positive or negative remodeling, plaque composition ( soft versus fibrotic or calcified... ). As a famous playwright and novelist in Brazil used to say: Unanimity is not smart!